GEORGETOWN, Ohio — Greg Canter tries buttoning up his white dress shirt, before finishing off with a black tie and white tuxedo jacket with black trim. But he cannot feel his right hand, cannot get his fingers to work, and has to ask his soon-to-be stepson for help.
The then-39-year-old shook off the numbness as carpel tunnel, since it runs in his family, and went on to celebrate the happiest day of his life.
It was Feb. 17, 2018 — his wedding day.
There are dates throughout his life that are seared into his memory. But what he did not realize is, that date and in that moment, his life was changing forever, or at least life as he knew it.
It was not carpel tunnel. It was amyotrophic lateral sclerosis (ALS) and doctors told him that he had 30 months to live.
“I thought there’s no absolute way it could be me. I’m healthy. I’ve never been to a hospital in my life. I’ve never been admitted into a hospital. I never had a broken bone. I’ve never really been sick. I’ve been active in sports… I mean, my whole life, just been healthy,” Canter said. “And that was the last thing that I would’ve ever expected on me.”
But his life would pivot once again, when in January 2019, he walked through the doors of a University of Kentucky medical clinic in Lexington, Kentucky. Maybe, he thought, this was no longer a death sentence for him.
That is because a new “breakthrough” treatment for ALS is showing signs of hope — and experts say, it could benefit other neurological diseases as well.
You might know it as Lou Gehrig’s Disease or remember it from its social media hype during the Ice Bucket Challenge in 2014, but for Canter and thousands of others, it’s a matter of life or death.
Between 20,000 to 30,000 people are living with ALS — a highly debilitative and progressive nervous system disease — at any given time in the U.S., and there are 5,000 new cases every year, said Dr. Sabrina Paganoni, an investigator and researcher at the Sean M. Healey & AMG Center for ALS at Massachusetts General Hospital in Boston.
“People with ALS have progressive muscle weakness, which means they progressively lose the ability to do many activities daily like walking, talking, swallow food,” said Paganoni, who is an assistant professor at Harvard Medical School and Spaulding Rehabilitation Hospital and has dedicated her career to studying the motor neuron disease, which affects nerve cells within the brain and spinal cord.
“The disease is rapidly progressing and fatal,” she continued. “It will involve other body regions, so the weakness will get more severe. ALS, oftentimes, strikes people in the prime of their life, so you have perfectly healthy individuals who might be in their 40s or 50s or 60s, who are actively working and living their life when the disease starts.”
ALS is ultimately fatal because it affects the diaphragm’s muscles, leaving patients unable to breathe on their own, Paganoni said.
“The (patient) will essentially lose control of the muscles in their entire body, including loss of control of the diaphragm, which is a muscle in our chest area that controls respiration. So, in order to breathe in and out, we have to use muscles,” she explained. “The diaphragm moves up and down with the muscle and that will allow the lungs to expand and breathe in oxygen and then release CO2. We don’t think of respiration as a process that is driven by muscles, but it is.”
Research has not quite pin-pointed the cause of the disease, however, in very few cases, it has been proven to be genetic, said Dr. Adam Quick, a neurologist at The Ohio State University Wexner Medical Center (OSU).
“It’s an interesting disease in that most of the time, it’s what we call ‘sporadic,’ which means it’s something that people get and we don’t know why — which is true of many diseases in medicine. We don’t know what is the thing that triggers it or starts it to begin with, and I think that’s true with most cases of ALS,” Quick acknowledged.
Only about 10 percent can be attributed to an abnormal gene, a family history of the disease, as the cause, said Quick, who has been researching ALS for 17 years, including 13 years at OSU, where he treats ALS patients. The remaining 90 percent of those diagnosed with ALS are considered “sporadic” or without a known cause.
Canter is part of that 90 percent.
In 2018, he started noticing a change in his body. The 38-year-old’s right side was weakening.
Although looking back, he said, he started having weakness back in 2015 while he was a school custodian. The sports junkie and avid basketball player — all the way back to his high school glory days for the Bethel-Tate High School Tigers — could not make a three-point shot as he always had before. He just chalked it up to getting older and losing his touch for the game.
Now, he said, he believes it was actually an early symptom.

However, by January 2018, his symptoms were undeniable.
While working in construction, he said, he noticed his right index finger and thumb “just quit working.” Over the next year, his right hand continued to lose dexterity and was progressively getting weaker, including in February on his wedding day when he had trouble buttoning his shirt.
Following his 39th birthday, Canter was required to get a physical for his CDL license. So, on Sept. 18, 2018, he went to the doctor for what he thought was a routine check-up and physical so that he could continue his job. But test results showed that he had blood in his urine and muscle atrophy in his right hand. He was promptly referred back to his general physician for further review and testing.
He will never forget the day his doctor uttered three letters into his ear.
It was Oct. 15, 2018.
“I walked in — three minutes. She didn’t touch me. I didn’t remove any clothing. She looked at my hands. Heard what the doctor told her where I came from,, and she goes, ‘ALS,’” Canter recalled.
“I’m like, ‘No.’It just threw me for a loop because the only thing I ever knew about ALS was the Ice Bucket Challenge back in ’14. I participated in it; my family participated in it. Nobody knew what it was. It was kind of like fun game.”
Later, in 2016, donations from The ALS Association’s Ice Bucket Challenge would finance part of the research for a breakthrough treatment with a $2.2 million grant, Paganoni said.
But for Canter, the game that raised money for throwing a bucket of ice over your head, turned into his new reality on Oct. 17, 2018.
“That’s how ALS hits you. Until it hits close to home, nobody really knows nothing about it. That’s why it’s so in-the-dark deadly,” Canter said. “There’s not enough knowledge out there for people.”
Two days after his doctor said those three letters to him, he saw a neurologist. After several hours and numerous blood, nerve and muscle tests, the specialist concluded the same fate for Canter.
“He called us into a little room, and he goes, ‘It’s ALS.’ I mean, here I am hoping he’d tell me I had brain cancer. I was hoping he’d tell me I had leukemia, because all of them options, you can fight them. ALS, it’s a 100 percent fatal disease; they consider it terminal. The average lifespan is 30 months with ALS. And just not knowing nothing about it, that’s really the last thing I wanted to hear,” Canter said.
“When he said that, I thought, ‘There’s gotta be a way he’s wrong,’” he said.
So, he went to another neurologist for a second opinion at The Cleveland Clinic in November 2018.
After four hours of tests, that specialist came to the same medical conclusion: ALS.
Following a third and final diagnosis from UC Health, Canter started rigorous treatment, including working with seven medical professionals to help him through the process, including occupational and physical therapists and a social worker. He was prescribed 23 daily medications, however, most of those drugs did not attack ALS, he said. They only eased some of the discomfort associated with the disease. But one of those treatments did include one of the only two FDA-approved medications specifically for ALS, riluzole — which his doctors told him would expand his life expectancy by a few months.
“At the time, you’re given a diagnosis, and I was told one to three years to live, if it extends me one day, then (it) worked.'”
Those first few days, weeks and months were a blur for the now-41-year-old, starting with three opinions all concluding with the same unconscionable diagnosis — and for him, he thought, was a death sentence.
But over time, Canter said, a few extra months was not enough.
“All of these people dying today, should be alive tomorrow in today’s world. ALS should not be a terminal illness in 2020,” he said with conviction and determination.
He wanted to do whatever it took to treat his ALS, to prolong his life, even if that meant being what he called, a “guinea pig.”
And while Canter was experiencing what he believes now to be early-onset symptoms, two college students were brewing up an idea inside their Brown University dorm room that would, again, change everything for Canter.
Changing Lives Inside a Dorm Room
More than seven years ago, 21-year-old Josh Cohen and 22-year-old Justin Klee popped the cork on a bottle of champagne to celebrate the beginning of the rest of their lives — that is to say, potentially saving lives.
While cure is a four-letter word they are not yet ready to use, the young pair believes their drug will advance steps in finding the right treatment combinations allowing those diagnosed with ALS to live longer, more functional lives.
In 2013, Cohen was studying bio-medical engineering and Klee was studying neuroscience at Brown University when they developed an idea out of what they called “scientific intrigue.”
Cohen remembered that early on in their planning stages, he was curious about the science behind neurodegenerative diseases and how best to treat them — going after the cells that are prone to stop working.
“What I ended up coming up with and linking up with Justin on, was an approach to make neurons more resilient — targeting a couple of key cellular death pathways in neurons and then the hope was that if you could keep these neurons alive longer, that it might treat some of these terrible diseases and allow patients to stay functional longer,” Cohen said.
“When we were just starting, I think we were excited about the science but we really had no idea what it meant; what it was going to require to start and build a company,” Cohen said. “I remember when Justin and I started it together, we cracked a bottle of cheap champagne and said, ‘Yeah, we’re starting a company. Here we go!'”
For Klee, who was personally touched by the effects of neurodegenerative diseases, it was a venture well worth the hard work that was about to mount for them.
“I certainly had in both sides of family — not ALS specifically, but one of my grandfathers had mixed dementia, as it seems most dementias are, we’re finding out. But actually, when we started the company, I had another grandfather who passed away from Parkinson’s,” Klee said. “We felt like these are really huge problems and everyone has had some family member, some person they know affected by these diseases, and we thought this was an approach people hadn’t taken.”
What really put things into perspective for them regarding ALS and how to treat it, was when they started working with doctors, like Quick and Paganoni, and putting faces to the disease while meeting with their patients — seeing what they deal with, with this disease on a daily basis.
“We just felt like, ‘My God, if there’s anything we can do to help, we have to do it,” Klee recalled.
And from that, CENTUR AMX0035 was born.
The longtime friends realized they worked well together and we able to tackle issues from each of their backgrounds in a unique way.
“We found from the beginning, in approaching problems, we found that we came at things in different ways,” Klee said. “Josh, with an engineering background, would think a lot about inputs and outputs and processes. Whereas, coming for a neuroscience background, I think I thought about things from a more biology-type approach. I think we found that that was really complimentary in developing the drug.”
“When we were initially starting out, I think even just getting things kicked off was the initial goal. I don’t think we ever foresaw that this would really get to clinic, get to patients. From the early days, we hoped that we could move it very quickly, but it has been a long journey,” Cohen said. “A long journey to clinic and a long journey to the data. I certainly don’t think we anticipated this would happen and I think we’ve kind of taken it step-by-step and we’re kind of shocked and feel very luck that things are where they are.”
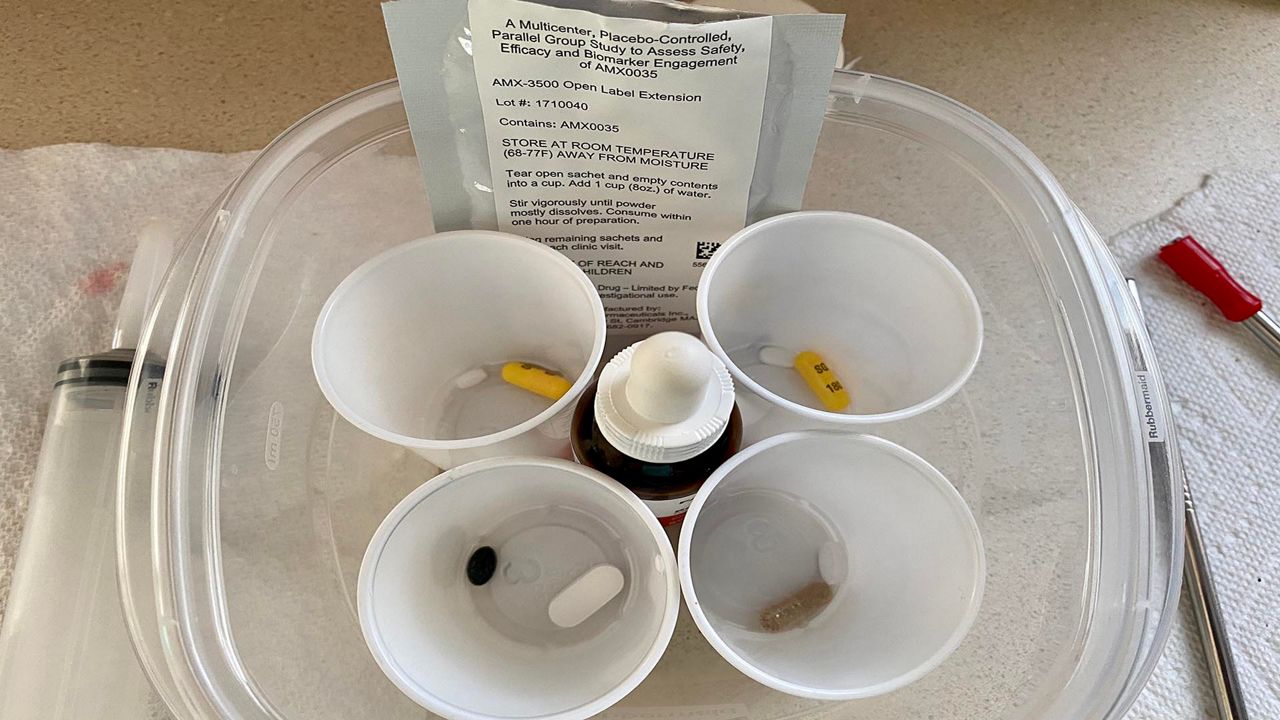
The drug, AMX0035, that comes in a powder-filled pouch that can then be dissolved in water for patients to take it orally, he said, is designed to target a couple of key cellular pathways that are involved in the cell’s decision to die.
“If you think of neurodegenerative disease broadly, these are diseases where we have a large amount of abnormal cell death,” Cohen continued. “So, our idea with the drug was if we target some of those areas where the cell is making the decision to die, we might be able to slow, or in the best case, stop nerve degeneration and allow patients to retain function longer.”
But to prove that AMX0035 was more than just a concept, Klee and Cohen, with the help of several doctors, clinics and medical experts, put together a clinical trial study to understand the drug’s effects and record its data.
“I think for a long time, and still to this day, we realized that going after Alzheimer’s, ALS, diseases that, unfortunately have a lot of clinical failure, that there would be a lot of skepticism, and that, honestly, we couldn’t be sure that this was a real therapy until we did the right tests — combined with our age and we weren’t seasoned bio-tech executives — so, it was really important for us to put as much of the money and our time towards research as possible,” Klee said. “We really wanted the science to drive things and see where it led.”
Canter, of Georgetown, Ohio, was on the hunt for anything to help his disease and its rapid progression creating a new physical obstacle for him every day.
“It’s a daily struggle when you can’t do what you used to do, and a lot times, what you could do yesterday. With ALS, that’s how everything is described: ‘Today is going to be better than tomorrow.’ Tomorrow is always worse than today. It’s a downhill roller coaster. You don’t get better from ALS. It’s not like other diseases, where you have good days and bad days. Every day is worse — every tomorrow is worse than today,” he said, sitting in his chair by the front door and wide picture window, resting his hands on the arms of his tan recliner.
He wears a medical alert bracelet on his wrist, layered with a red rubber bracelet with bold white letters: #ALS Strong, leading to his fingers and hands which now curl under.
“I wouldn’t give ALS to my absolute worst enemy in life because I know how bad it is, and I wouldn’t give that to anybody,” Canter said.
These days, he cannot walk on his own, he said, using an electronic wheelchair or walker to get from room to room. He struggles with everyday tasks like standing and picking up items like a 2-liter of pop.
“I have the strength of a 2-year-old kid,” he explained. “The easiest way to explain it is, a full-body paralysis from head to toe. The only muscle it doesn’t affect is your eyes.”
“Your nerves die in your body and when your nerves die, the muscles that react to your nerves, when the muscles aren’t getting used, they eventually dissipate; they eventually waste to where you’re skin and bones,” Canter explained. “I’ve got no pain. No pain at all on my body. I don’t hurt. It’s just that my legs get so heavy; it’s just the weakness and the muscle dying. That’s the problem with it. It’s a silent killer.”
But the effects on his life, he said, are more than physical. He feels like a burden to those who love him.
“You require help, that in the years prior, you never needed — where people have to change their lifestyle, to make your lifestyle. So, it doesn’t just affect you, it affects the ones around you,” Canter said.
His mom and dad, who live about 20 minutes away, drive to his house twice a day, once at 12:30 p.m., for lunch and medicine, and then again to make him dinner and more medicine around 6:30 p.m.
He has had to put away his pride, he said, and accept their help. But that was not an easy task.
“You need to ask for help. You don’t need to suffer,” he said he was told by others he met with ALS. “It means everything. You learn who’s there for you, who’s got your back and who doesn’t.”
But more than a burden, he said, “It’s an emotional toll that it puts on everybody. They see me dying because of going downhill.”
“You never appreciate your body, your hands and legs. You take all that for granted when you have it. Your legs and your arms and your hands are valuable pieces. You never want to lose them. I mean, that’s a key component of life — and that’s what ALS does, we lose them, lose the ability.”
And Canter was ready to fight his disease that was taking away his ability to live life like he used to.
In 2019, he applied to join the AMX0035 clinical trial based in Boston.
But to enter a clinical trial, he had to prove his breathing capacity was at a vital level that was acceptable for the taking the medication. After blowing into an apparatus, he kept falling short by one point for breathing and could not get into the study.
He finally blew a 60 percent and was accepted into the clinical trial in January 2019 through one of the participating clinics at the University of Kentucky.
While it was a blind study, he believes that he received the placebo during the trial because his breathing deteriorated while taking his treatment.
But that would change following the initial trial study.
Trial Results, Pending FDA Approval
The 24-week clinical trial was studied in clinics across the country, like the one Quick runs at OSU and included 137 participants, like Canter. What they found is considered a medical “breakthrough” in ALS treatment, both Quick and Paganoni agree.
“People who received the drug in the trial did better than those who received the placebo,” Paganoni concluded.
In fact, she said, participants on the drug regained physical functions like walking and talking for longer than those without the drug. And ultimately, the outcome of the trial data indicated that it slowed down the progression of the disease.
“We were not able to completely stop and we were not able to reverse the disease, but it is certainly a fantastic step in the right direction. We still have a lot of work to do to really find a cure — something to completely stop or reverse the disease,” said Paganoni, who investigated the drug in an academic setting and helped design the trial and obtained funding through the ALS Association and ALS Finding a Cure, from part of the money raised during the Ice Bucket Challenge in 2014.
Paganoni has been studying and researching ALS for a decade and has been part of the research team on this trial for the past five years, alongside several medical colleagues.
“This is really a hopeful time in ALS research. We’re testing more drugs at a faster pace and we’re making more progress than ever. I’m really convinced that we’re just at the beginning of a new era in the discovery of new treatment for ALS,” she said. “This is definitely a great step forward; something that means that we are making progress, that we’re making a dent — that this in a way, hopefully, just the beginning of many more new treatments for ALS.”
AMX0035 is not currently available for prescription to patients outside of the trial because it is still being investigated at this time and awaiting FDA approval. However, what Paganoni saw in a relatively short amount of time over six months, she said, was that the drug slowed down the progression of the disease, and those findings were published by Paganoni and several other researchers in The New England Journal of Medicine in September.
“As a researcher, I find the data compelling and in addition, it really changed the tone of my conversations with patients. We spend our days talking to people and families about ALS and what it looks like, and now we can talk to patients with more hope. It’s hopeful day; we’re making a dent. We’re just at the beginning of a new era in the discovery of new treatments and so we need to continue in this line of work and continue to do more research, more clinical trials, until we find cures for everyone who has ALS,” she said. “This is the first step.”
In her role, Paganoni has continued to follow and analyze the trial data, including new data from an Open Label Extension of the drug for those patients who participated in the clinical trial, who are continuing to take the medication longer term, giving Paganoni more insights into the drug’s ongoing affects on ALS patients. She hopes to publish some of those results in the coming weeks, moving the FDA approval process one step closer to prove its function and capability to patients.
At this point, ALS treatment, she said, includes a combination of medications and therapy.
“ALS is a complex disease and if we look at other diseases that are complex, like cancer or HIV, or even heart disease, it’s really combination treatment that works. There isn’t any single drug or intervention that’s a cure… we’re not able to stop; we’re not able to reverse the disease yet, but every positive trial result, such as this one, really brings us closer to having more options and really, ultimately, having a cure,” Paganoni said. “We’re starting to develop new options to allow people to live better and that’s just the start of it, and I hope that it is just the beginning of a new era in the discovery of new treatment for ALS.”
Quick agreed that this could be just the beginning for more breakthroughs in ALS treatment.
“The bottom line was, the people who got the treatment, their progression or they’re worsening on that functional rating scale was slower than people who got the placebo,” said Quick, who was the director and investigator for the clinical trial at OSU, including some of his own patients.
While Klee and Cohen acknowledged that the effects could be different for each patient, what they saw in the trial and from its subsequent data from researchers like Quick and Paganoni, was that this drug could be the difference between “the ability to walk on your own or be in a wheelchair. It could be the difference between being able to feed yourself or needing a G-Tube,” Klee said. “I think the overall picture was that many patients kept their strength longer, kept their breathing longer.”
But, he said, they need to keep moving the needle forward on this drug.
“ALS doesn’t wait and we need better treatments, and what the data showed in our trial is that every day a person’s on therapy, matters. It means that they keep their functioning and abilities longer — and that could mean all sorts of different milestones in someone’s life. I think, while it’s exciting to have good data, at the end of the day, this is about people and families living with a really tough diagnosis that’s been unanswered for far too long,” Klee said. “While we’re excited, we now feel more of an urgency than ever that we need to get this to people.”
There are currently two FDA-approved ALS medications on the market that also show clinical benefits, including the one that Canter has been taking since his diagnosis. Rilutek (riluzole) was approved by the FDA in 1995 and Radicava (edaravone) was approved in 2017. Both have similar benefits to CENTUR AMX0035, Quick said. But together, he is optimistic that they could create a life-extending combination for patients.
“I’m hopeful that five years from now, we’ll have, maybe a cocktail of different things that we can give to somebody. And maybe each of them works in a slightly different way and together, they can kind of be combined to be something that will have a significant benefit in slowing down the progression of the illness,” Quick said.
However, he said, there is not one single medication on the market that stops ALS completely — but, he continued, AMX0035 does have a different mechanism of action in terms of the way that it works in the body compared to the previous two medications.
“It has a different mechanism of action, so it works in a different way on the underlying pathology of ALS,” Quick said. “In a lot of ways, it’s also similar to a lot of things we have right now — all of these medications work to slow down the progression of ALS. So, people who have ALS, even if we put them on these medications, they still get worse over time; the disease does still progress. But these medications slow down that process and delay it or spread it out over time, so that people on these medications stay at a higher level of function typically for a longer period of time, and it also delays that progression of the disease and helps people live longer.”
“At this point, anything that clearly shows slowing of progression with ALS, would be considered breakthrough because if you look at the history of clinical trials for ALS for the last 30 years, lots of things have been tried… and found to be not effective,” he said. “In a sense, that’s sort of a big breakthrough in that this is one of three medications over that last 30 years that has been studied that clearly [shows] some benefit in slowing down the progression of the disease. It’s a milestone.”
Quick said, ALS treatment will require a “multi-faceted approach” for what he called a “daunting problem” they are facing.
“There’s still a lot about ALS that we don’t know and there’s so many things going on in the nervous system with ALS,” he said. “I don’t think it’s going to be like one medication that you’re going to be able to give to people and that’s going to arrest the disease. It’s just a really complicated illness… and if you think about the world of cancer, in cancer you’re trying to kill cells. So you have these bad cancer cells you’re trying to figure out something that’s going to go into the body and kill those cells and make them dead, so that your cancer goes away. When we’re talking about ALS, we’re talking about trying to keep cells that are sick and trying to die and trying to keep them alive — and that’s a much more challenging problem.”
Paganoni concurs that AMX0035 is another strong tool for those combatting ALS and could be part of the right combination to save lives — something that she thinks could be right around the corner.
“These two options are a combination of medications to slow down the disease’s progression, and in addition to supportive care, there are the first building block. Now, with this trial we are adding another tool, at least a promising tool — again it’s still in investigation and we don’t know if or when it could be approved, but it means that we are making some progress, that we are moving forward and I think that’s hopeful for people with ALS,” she said. “Looking at the progress that we’re making and looking at the fact that we’re testing more drugs at a faster pace, I think really, the future is going to be brighter because we can make progress faster. We have a very cooperative, a very active research community.”
“The pace is accelerated… it is the time to learn about ALS research [and] continue to do ALS research,” she continued.
With extended research and more medications to treat the symptoms, and potentially slow ALS’s progression, Quick is confident that they are on the cusp of more medical breakthroughs — and that is, in part, thanks to this new treatment discovered inside a college dorm room.
“We’re starting to see things in the pipeline of treating ALS that have a really good rationale for using them, and different medications that work on different aspects of the disease,” he said.
While there was a 25-year gap in breakthrough treatment, from 1990s and 2017, Quick said he hopes to see a new medication in research every year or two from here on out.
“I’m hopeful that we’ll start to see this process of maybe every year, every other year, we start to find a new medication that has some effect on slowing down the progression. I’m hoping that’s where this is going and it’s not going to be another 20 years before we find something that’s effective.”
With that, he is hoping in the next five to 10 years, they will be able to offer a more effective combination of treatment for ALS patients.
“This was a success and it was really one of the first successes in a treatment looking at a disease like ALS which is a very difficult-to-treat, challenging, neurodegenerative condition that really showed an effect. Our understanding of the nervous system getting better and better, I think we’re going to start seeing more and more things like this that are going to have some effect on these really difficult-to-treat neurodegenerative conditions, just as science gets better and we learn more about these illnesses,” Quick said. “I think it makes patients more hopeful when they see a lot of research is really being done very actively in this and that there’s a lot of interest in it, and there’s a lot of ongoing studies to be a part of. I think it does change the conversation quite a bit when I’m talking to people about this. It’s still an incurable illness but it’s not an untreatable illness.”
For the two guys who cooked up this idea in a dorm room, the results were something that they could never had anticipated.
“In ALS, trials have been going on for decades, and very, very, very few have been successful. So, I think whenever there is a successful trial in ALS, it’s a big cause for celebration. I think it is a breakthrough against the disease,” Cohen said. “I kind of see this as just the beginning and hopefully the first drug of many that will continually make the quality of life and the state of this disease better and better. Unfortunately, steps like this have been few and far between and we are really excited that a breakthrough like this happened.”
“It was incredibly thrilling and kind of fulfilling and inspiring… but I think also a very heavy sense of responsibility that it’s now on us to work closely with regulators and get this drug forward as fast as possible,” Cohen said, who along with his partner, is working on federal drug approval through ongoing discussions with FDA and regulators worldwide, including in Canada, Japan and Europe.
For the inventors of this medication, it is important to maintain momentum because every second counts.
“We got all of the data at one moment at the end when the study was complete and getting that data’s pretty thrilling — also, quite stressful. But we were over the moon when we saw it was positive,” Cohen said. “I think it pretty immediately also set in a pretty strong feeling of responsibly that once we have this data that patients with this rapid and progressive disease, really have no time to wait, and that every minute, every hour, that we’re spending, we need to be spending to move it faster. We can’t lose time at any juncture.”
While not a cure, perhaps one of the most notable breakthroughs is the optimism gained from the trial.
“I think the other thing is, this data injects a tremendous amount of hope into the field, and optimism, and I think that’s really important because I think it reinvigorates all the research efforts that’s going on. It gives a new handle and lens by which to understand the disease because we can ask, ‘Why exactly did this drug work and are there insights we can take from that to treat the disease even better?'” Cohen said.
Not long after the trial, some of the researchers and staff threw a surprise party for Klee and Cohen, and one of the nurses walked over to them and told the pair something that has stuck with them.
She said, “My job every day is to talk with patients and families and tell them the worse news. I tell them they have a death sentence and I tell them how they can deal with it and I tell them what’s going to happen and it’s my daily job. I do that every single day; I’ve been doing that every single day for over 20 years. This is the first day, that I could tell them all there’s hope.”
“That was one of the moments where it really hit it home. It’s easy for these things to be data on a page or science in a paper, but it really hits home when you realize that every data point, every statistic are people when you’re going through this. So, I felt incredibly humbled, and definitely feel a big responsibility going forward,” Cohen said. “There’s progress. There’s hope.”
With the success in ALS treatment, Klee and Cohen, co-founders and co-CEOs of Amylyx Pharmaceuticals, believe that their “breakthrough” medication, CENTUR AMX0035 could be a proof of concept for other diseases, and they hope to get more studies up and running in those areas as well.
“The goal of the therapy was intervene in the neurodegenerative process, so it’s not necessarily specific to ALS,” Klee said. “We think that the drug could benefit in any disease where neurodegeneration is an issue, and there are many of them, Alzheimer’s, Parkinson’s, Huntington’s.”
Quick believes, thanks to AMX0035, this could be just the beginning for more medical breakthroughs.
“I think that neurological diseases are one the next big frontiers in medical science because they are challenging and for a long time it was a tough target to go after. I think we’re understanding so much more about the nervous system than we did in the past but I think with the right resources, I think we’re going to be able to learn a lot more and be able to come up with things that are not just going to be better for treating ALS but be better for treating things like Parkinson’s disease and Alzheimer’s disease and Huntington’s disease and multiple sclerosis, so I think we’re kind of at the cusp of, what is hopefully, an explosion of new treatments and better understanding of these neurological conditions that have been historical hard to manage and treat,” Quick said.
In fact, the drug is currently in a clinical trial for Alzheimer’s and Cohen and Klee continue to evaluate a number of other neurodegenerative diseases that could benefit from this therapy as well. In the next year, they are hopeful that their Alzheimers trial data will be released, in which they are using the same dose of AMX0035 with a 100 participants.
But as for ALS, while it may not be a cure, it is the next step towards that four-letter word.
“I think what’s easy to forget sometimes, is that we all want cures and that’s what we need to work towards. But if we look at the development in diseases like, HIV, cancer, the first therapies weren’t cures, but they were breakthroughs. They said, ‘We can treat this thing.’ And now, look where we are. I mean, diseases that were death sentences are now being treated as chronic diseases and sometimes can be true cures. That’s what we want in ALS, too,” Klee said. “This isn’t a cure, but we do think it’s a breakthrough. And the reason I wouldn’t say, ‘miracle,’ is because like all things in medicine, you have to ground things in really deep science. And we were so fortunate that we had this good idea but then we had some real leaders in science and medicine help us to get to this point. I think the biggest takeaway is that the drug benefited people. We tested it in the best clinical centers in the country and we ran a really rigorous trial and the drug showed benefit. It’s not a cure but it’s a big step forward and we hope it’s just the start.”
Cohen agreed.
“I think this is a really hopeful time in ALS,” Cohen said. “We’re hoping that the landscape of this disease and the shape of this disease changes rapidly over the coming years.”
Their drug has already changed the landscape for one man: Canter.
“Us, who’s suffering from ALS, we’re not looking for a cure right now,” he said. “Before you have a cure, you have to have treatments. I’m lucky, because I was in the trial, but there’s thousands suffering with nothing.”
And he wants to help be the voice for other patients who are suffering from the terminal disease — in hopes that one day, the word, “terminal,” can be dropped from its diagnosis.

Following the 24-week clinical trial, Canter was given the option to join the Open Label Extension trial for the drug, giving him the opportunity to knowingly take CENTAUR AMX0035 for researchers to study the long-term impact of the drug.
Since Canter started taking the drug regularly outside of his initial trial phase, he said that he has already noticed the progression of his ALS symptoms change.
“I started noticing my breathing pattern… it drastically slowed down my progression in my breathing pattern — in my lungs, my diaphragm,” he revealed.
However, his extremities, like his hands, arms, legs, have steadily gotten weaker.
“I’m not saying I’m getting better, but that shows me that my breathing, which you have to have to live, has really seen a positive reaction to this medicine, drug I’m taking,” he said.
Like Canter, 90 out of the original 137 participants have opted to continue into the Open Label Extension, giving him and others something that they never thought was possible with ALS: hope.
“One thing you have to have in life is hope. And this medicine gives me my hope right now,” Canter said. “There’s hope right around the corner.”
He will be guaranteed the medication from the trial, he said, until May 2022.
But the early idea he had of gaining one more day, or even a few more months to live, when he was first diagnosed, has since changed.
“I want years,” he said. “I think if it wasn’t for this drug, I would be in the ground today. I think this drug is keeping me above ground as we speak.”
But waiting on the FDA to approve the drug he believes has helped him already, frustrates Canter.
“In 2020, with all the help that’s out there, these people that are dying today, should still be alive tomorrow, point blank. Give us the help that we need. The help is out there. It’s not fair,” he demanded. “Give us access to these treatments. ALS isn’t what’s killing us. ALS isn’t the battle; it’s getting these approved and assessable to all.”
While Canter said ALS has long-been known as the “cry-and-die” disease, he refuses to give into that theory and plans on fighting for his life.
Acknowledging that you seldom hear of success stories with ALS, Canter said that he is determined to be one of those rarities.
Unlike most ALS patients, Canter has not yet lost his ability to speak. And he uses that to the fullest, not only for himself, but to amplify his voice on behalf of anyone else battling this disease.
“I’m lucky to still have a voice. So many people with ASL don’t even have a voice anymore,” he said. “So, when I speak, I speak for them, for the ones who can’t talk.”
While there is no cure for the fatal disease, Canter has something he never thought possible back in 2018 when he was first diagnosed.
“You have to keep hope. We’ve got help right around the corner. You can’t give up,” he said. “All these people are suffering… and in a matter of one day, something could be changed.”
Bucket List and Blessings
Sitting inside his quaint white house, situated on a slight hill in his small, rural town in Brown County, Canter grips tightly to his independence for as long as he can. In the kitchen, next to a Cincinnati Reds face mask, sits a large, blue pill box inside a woven basket, filled to the brim with his medications for the day.
The man who once considered himself a healthy athlete, is now confined to his recliner next to his front picture window, where we watches the world moving on around him — neighbors going about their daily lives — driving to work, doing yard work, enjoying life. Next to him, on a wooden T.V. tray, is a container of his afternoon medications in small cups and pouches that his mom has put together for him because he cannot do it himself.
“If you would’ve asked me two years ago what paralysis feels like, it was nothing like what I’m experiencing. I always thought that like, your mind has control of your body to where you could look at hand and say, ‘Open up, hand!’ It’s attached to you and how it’s all attached to your brain, and no matter how hard it is, you can always get them open. Well, it doesn’t work that way. Like, my right thumb is dead. I’ve got nothing in my right thumb — I can’t bend it or nothing, no feeling. It’s like it’s not even attached to me anymore,” Canter said.
It is a frustrating obstacle, but he has learned to overcome what his body can no longer do.
“You learn to cope. You learn to adjust your life,” the once-avid hunter said, sitting in his living room where two of his prized deer trophies are proudly mounted on the wall behind him.
“You learn to adjust your abilities and you live today with what you’re given. I’m just so thankful that I’m here.”
To further cope, he likes to remember that “blessings still happen every day,” he said wearing a camouflage trucker’s ball cap, donning an American flag.
One of those blessings is just outside.
In his slanted driveway, sits a handicap-accessible van — but on the other side of his two-car garage door is his ticket to the outdoors and his independence.
As the motorized door rolls up, a polished, but dusty, bright yellow Corvette sits parked. He has not taken that out for a ride in more than a year. These days, he revs up a different ride for cruising, his scooter — and it has made all the difference for him and given him the ability to feel the fresh air on his face and the wind in his hair.
“You sit inside here, this is what kills people. Sitting in a chair in a quiet house, alone, where your mind races and tries to wonder off on you. That’s what kills you,” Canter said. “Being outside and become active, and even with my abilities, I still like to ride my scooter.”
His dad helps him onto his scooter, but once he is perched on his three-wheeled Harley Davidson scooter that tops out at 12 m.p.h., he has a 45-mile range to ride freely.
“Fourteen miles, one day I rode it. That’s my mind therapy. When I can do things outside, that’s a huge bonus, a huge help — keeps me from thinking,” Canter said.

According to the ALS Association, someone is diagnosed with the ALS every 90 seconds. Johns Hopkins Medicine estimates that disease is responsible for as many as five out of every 100,000 deaths.
“We’re all dying. In a way, we’re all terminal… in reality, nobody knows what your expiration date is; everybody’s got one,” Canter said. “From the beginning, it’s a life sentence when they give it to you. You know you’re not going to have much of a future left.”
But he was determined to make the most of his life, regardless of his “expiration date.”
When he was first diagnosed, he remembered, his doctors told him, “My future is now. If I have a bucket list, work on bucket list now… basically, you’re living for today. If there’s anything in life you want to accomplish, do it now, while you can. That’s how everybody should be living anyway. Nobody’s guaranteed tomorrow.”
For him, that started with taking in every Reds baseball game he could — which led to a pretty special day at Great American Ballpark last year.
On May 5, 2019, the Cincinnati fan was named the captain of a home game against the San Francisco Giants. Even though he could not throw out the first pitch, he did take the starting lineup to the pitcher’s mound, where he was announced and his story about ALS was told to the fans, who, in turn, gave Canter a standing ovation.
“It was a very neat experience,” he said, remembering it only by watching video from the day, because he was too awe-struck from the sheer excitement of it all.
Continuing his bucket list and his Reds-fandom, Canter took a road trip following the team’s season, traveling to ballparks in Milwaukee and Chicago. Along the way, he met several Reds’ players and still keeps in touch with them today.
“I’ve had so many people come into my life because of this illness, that I could have easily just kept my eyes shut and my heart shut and not let them in my life — and that has been so valuable in the past two years to me,” Canter said.
He keeps them close these days because, he said, he gains power and immeasurable strength from those around him.
“When you surround yourself with negativity, you’re going to become a negative person,” Canter surmised. “When you surround yourself with positive people and positive influences, you become a positive person; it’s contagious.”
From that positivity, he builds up his own motivation to power through and overcome ALS or whatever comes his way.
“Inspiration and motivation is a power that you build inside of you. It’s not given to you, you have to find it,” he advised to anyone struggling.
And Canter is inspired to keep moving, however he can, and counts his blessings for the treatment that has already shown signs of promise.
“No matter how bad ALS is, there’s still blessings that happen every day,” he said. “You just have to have your eyes and your heart opened up to see it and accept it.”
The ALS Association has a petition online for FDA approval for the drug, AMX0035. To learn more about ALS, donate to ongoing research and to sign the petition, visit https://www.als.org.